With the change of seasons, it seems that the state of our people changes. One of the manifestations in the skin is that some people will experience peeling of the hands and feet.
What's wrong with peeling skin? The answer is not so simple, because there is more than one possible skin problem, and the cause is not necessarily just the "change of season".
Today, we will focus on a few common problems that can accompany hand/foot peeling - exfoliative keratosis, sweat pimples, juvenile metatarsal dermatosis, chapped skin and ringworm.
I. Exfoliative keratolytic disease
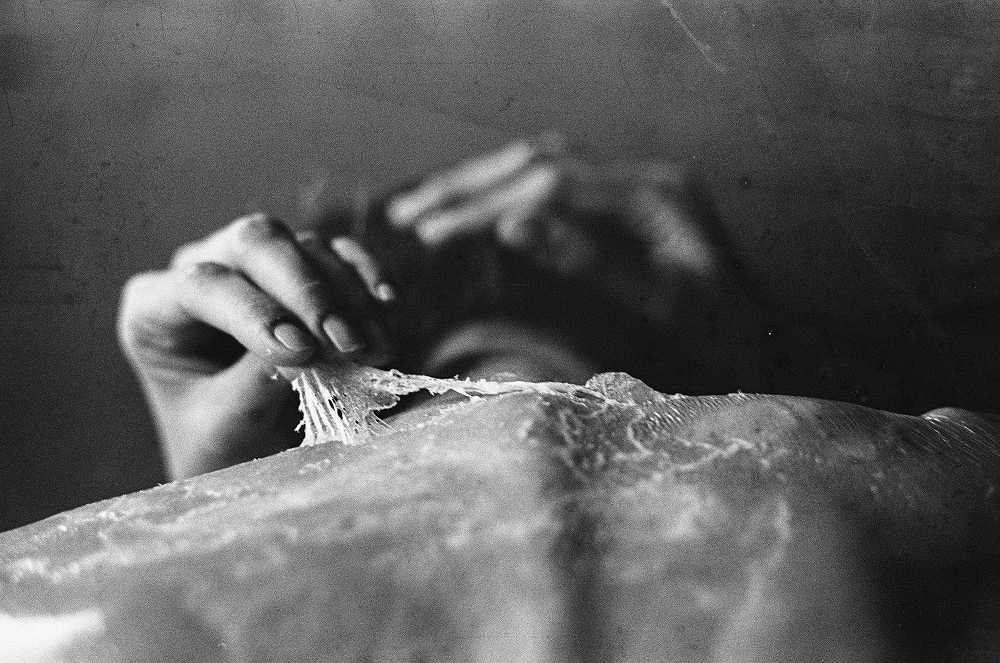
Exfoliative keratolytic disease, which sounds very academic, is actually mainly manifested as peeling of the skin on the hands (sometimes including the feet).
It tends to recur, and may worsen especially when the weather is warm, rubbing, or touching water.
The cause of its appearance is unclear; some believe it is related to sweating [1], while others believe it is related to eczema or fungal infection [2], although it is not an infection per se and is not contagious to humans.
Specifically, exfoliative keratolytic disease has the following characteristics [1,2,3].
✔ It is more common in the youth group, although it can also occur in other age groups.
✔ Predominantly on the palms of the hands and/or soles of the feet, including the fingers and toes.
✔ The disease is mild, usually not itchy or painful, and is easily accompanied by sweating.
✔ There is thin, round or patchy peeling of the skin, which may be accompanied by slight redness and air-filled blisters.
✔ Can be cured without treatment, but may recur in the future.

The main point of treatment for exfoliative keratolytic disorder is to find and avoid triggers and aggravating factors. Moisturizing, if done, may be helpful. Other than that, medication is usually not required for treatment.
II. Herpes sweat
Eczema is a type of eczema, which can also be called dysphagic eczema. But its cause is not very much related to sweating, which is a misnomer.
Theoretically, its causes are physical, exposure to irritants or allergic substances, and individually, it is also related to mental stress [4].
The reality is that many people cannot find a specific cause and go back and forth for months or even years, and are especially prone to relapse during warm weather.
Specifically, herpes sweat is characterized by the following features [4].
✔ It occurs mainly in the young population and is less common in the pediatric population.
✔ The first stage is mainly blisters and intense itching, with deep blisters (not easily broken), a large number of them, of different sizes, and easily occurring on the sides of the fingers and palms (sometimes on the soles of the feet).
✔ There is peeling in the later stages, which occurs after the blisters have dried and absorbed. There may also be keratin thickening and cracking if there are frequent recurrences.
✔ Usually heals without treatment within a few weeks, but is prone to recurrence in the future.

The main points of treatment for sweat blisters are to find and avoid the cause and aggravating factors, to control skin inflammation and itching, and to take daily care of the skin to reduce skin irritation. The specific medication regimen varies from person to person (especially the severity of the disease).
III. Juvenile metatarsal dermatosis
Juvenile metatarsal dermatosis is a rather characteristic skin problem, but not many people recognize it.
The word "metatarsal" here refers to the area where the disease is most likely to occur - the soles of the feet.
The nature of juvenile metatarsal dermatosis is similar to eczema and may be related to the body type, but in many cases it is also related to local factors, such as the physical and chemical effects of shoes, synthetic fibers, friction, sweating, etc [5,6].
Specifically, juvenile metatarsal dermatoses have the following characteristics [5,6].
✔ Commonly seen in children aged 3 to 14 years, especially in the age group of 4 to 8 years.
✔ The most common sites are the anterior aspect of the soles of the feet, the underside of the toes and the weight-bearing areas of the soles of the feet, with the toe seams largely unaffected.
✔ The prominent manifestation is localized patches of dryness, redness and shine, with secondary manifestations of peeling and cracking.
✔ Usually not itchy or painful, or painful if cracking is evident.
✔ Can heal without treatment and may recur annually in the short term, although most will subside in adolescence.

The main points of treatment for juvenile metatarsal dermatosis are to avoid the local disadvantages mentioned above and to apply topical moisturizing products.
If necessary (if redness and itching are evident) topical glucocorticoid creams can be applied. If the skin is visibly cracked, limit strenuous activity for a short period of time.
IV. Cracked skin
Many people (especially adults) have heels (and some hands) peeling, thickening, cracking, according to the form we can generally be called skin cracking.
The cause of cracked skin varies from person to person. If it is simply a heel problem, it may be related to physical and chemical factors such as wearing open heel shoes, using soap, dry skin, dry climate, and prolonged standing.
Individually, other skin conditions (e.g. eczema, tinea pedis) may also accompany chapped skin.
For common chapped skin, it has the following characteristics [7].
✔ There is usually only a superficial skin problem, such as peeling, thickening and cracking, without manifestations such as patchy redness, oozing and blisters.
✔ There is usually no itching or pain, or pain if cracking is evident.
✔ May improve spontaneously, or may persist for a long time, or worsen in specific seasons.

The main point of treatment for chapped skin is to apply moisturizing products thickly, in addition you can choose products that soften the keratin (containing urea, salicylic acid, etc.).
Daily attention is paid to local protection, choosing comfortable shoes, insoles and socks, reducing frequent mechanical wear and chemical stimulation, and avoiding dry skin [7,8].
If skin cracking is severe or there are other abnormal manifestations of the hands and feet, medical evaluation and disposition are required.
V. Tinea capitis
Tinea versicolor is a fungal infection that may be contagious to each other. However, the most common type of ringworm is tinea pedis, commonly known as foot fungus.
The fungus that causes tinea pedis feeds on the keratin of the skin, destroying the surface layer of the skin while causing an immune response to the skin, which results in peeling, redness, blistering, and thickening, usually accompanied by itching.
Specifically, tinea capitis has the following characteristics [8].
✔ It is most prevalent in adults and adolescents, and is less common in prepubertal groups.
✔ The more typical form of tinea pedis is "rotten feet", which refers to peeling, whitening, blistering, and itching of the toe crevices. The most common toe stub is the little toe stub.
✔ Some tinea cruris are characterized by thickening and peeling of the skin and tend to invade the soles, sides, and heels of the feet; others are characterized by clusters of blisters that tend to occur in the center of the soles or at the ends of the toes.
✔ Tinea corporis is usually only unilateral and is mainly a peeling, thickening of the palm of the hand.


The most targeted treatment for ringworm is the use of antifungal medications, and topical creams are usually sufficient.
Since fungi are highly adaptable and contagious, daily care of tinea pedis (dryness, breathability, avoidance of infection, etc.) is also important, otherwise the condition tends to recur.
It is important to emphasize that there are many different types of skin diseases and not all problems that can cause peeling of the hands and feet are listed here. If you are not sure of the diagnosis, or if you do not know the details of the treatment, you should see your doctor and deal with it formally under his guidance.